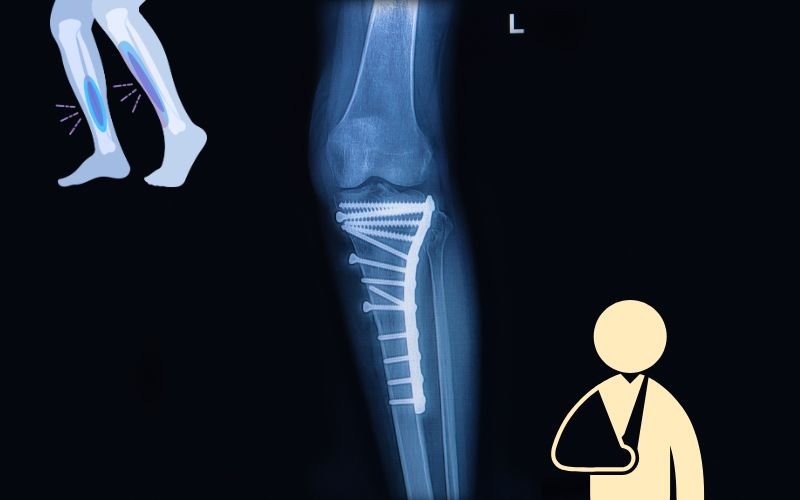
Did you know that the tibia is the most commonly fractured long bone in the human body? According to data from the American Academy of Orthopaedic Surgeons (AAOS), tibial shaft fractures alone account for more than 500,000 orthopedic injuries every year globally, with a disproportionately high number reported in active individuals and accident victims. In India, due to the sheer volume of road traffic accidents, averaging over 4.6 lakh cases per year, the incidence of tibia and fibula fractures continues to surge, especially among young adults and the elderly.
But here’s the critical detail most people overlook: a tibia fracture is never just a broken bone. When the fibula is involved, or when the break occurs near a joint (as in proximal tibia fractures), it becomes a complex biomechanical and surgery challenge.
Dr. MS Bajaj, one of the most respected orthopedic specialists in Indirapuram, Ghaziabad, and across UP, with a reputation for handling everything from simple tibia fractures to complex tibia-fibula combinations and joint-sparing proximal tibia surgeries offers the kind of expert care that restores lives.
In this comprehensive guide, you’ll discover everything you need to know about tibia and fibula fractures:
Tibia and fibula fractures
Tibia & Fibula
The tibia, often called the shinbone, is the second-largest bone in the human body after the femur (thigh bone). It runs from the knee to the ankle and bears nearly 85% of your body’s weight every time you take a step.
When it breaks, especially in the middle shaft (called a tibial shaft fracture), the structural integrity of your leg is compromised. That’s why tibia fractures almost always lead to immediate loss of mobility and extreme pain. There is no such thing as a “minor tibia fracture.”
Running parallel to the tibia is the fibula, a thinner bone located on the outer part of the leg. It doesn’t carry much weight, but its role in lateral stability, ankle support, and muscle attachment makes it essential.
In many high-energy injuries (like bike accidents or sports injury or trauma injury), the tibia and fibula break together. This is called a tibia-fibula fracture, and the damage is more complex. When both bones are fractured, it’s becomes a task of rebuilding the entire lower leg’s stability and function.
Why These Bones Fracture Easily?
Unlike the femur, which is set and surrounded by large muscles, the tibia is close to the surface which means it’s more exposed to external force. This makes it more vulnerable to:
- Direct trauma (road accidents, sports injuries)
- Twisting forces (especially in older adults or osteoporotic patients)
- High-impact falls
- Heavy object impacts in industrial settings
Proximal tibia fractures (near the knee) are particularly serious because they involve the knee joint surface leading to risks of arthritis, instability, and long-term stiffness if not treated correctly.
Fracture location also determines the complexity of treatment:
- Proximal tibia fractures (near the knee): Often intra-articular, may affect joint motion and weight distribution.
- Tibial shaft fractures: Most common; disrupt the main weight-bearing column of the leg.
- Distal tibia fractures (near the ankle): Affect mobility, gait mechanics, and ankle function.
Each location requires a different surgery, fixation technique, and rehab, something only an experienced orthopedic surgeon in Ghaziabad like Dr. MS Bajaj can evaluate with confidence.
Types & Classifications of Tibia and Fibula Fractures
A break in the tibia can range from a simple crack to a complex, joint-threatening injury. Let’s decode the common types of tibia and fibula fractures, where they occur, and what each one implies for treatment and recovery.
1. Tibial Shaft Fractures
This is the most common type of tibia fracture, caused by high-impact trauma such as road accidents or falls. It occurs along the mid-portion of the tibia, which is a critical weight-bearing zone. It can be displaced (bone fragments move out of alignment) or non-displaced, may occur with or without fibula fracture
Misalignment or delayed healing in lead to long-term gait abnormalities and chronic pain.
2. Proximal Tibia Fractures (Tibial Plateau Fractures)
These occur at the upper end of the tibia, near the knee joint. It Is caused by high-energy trauma or falls in older adults with weak bones. It can be intra-articular (involving the joint surface), which makes them more difficult to treat. This is classified further into lateral plateau, medial plateau, or bicondylar fractures and require ORIF (Open Reduction Internal Fixation) with plates and screws to restore the joint surface.
Improper treatment can result in post-traumatic osteoarthritis, chronic knee instability, and loss of mobility.
3. Distal Tibia Fractures (Pilon Fractures)
It is located near the ankle, these fractures affect the bottom part of the tibia, sometimes extending into the ankle joint, may also accompanied by fibula fractures. It is typically require surgery fixation followed by staged rehab. It may involve external fixation if soft tissue is compromised,
Delicate blood supply and risk to ankle joint make treatment challenging. Delay or mismanagement can severely impair walking ability.
4. Tibia-Fibula Fracture (Combined)
When both bones break in the same leg, the injury becomes exponentially more complex. This combination occurs in high-force trauma, and can be closed fracture, skin intact or open fracture, bone pierces the skin, increasing risk of infection or comminuted fracture, bone shattered into multiple pieces.
Stabilization must account for both bones. It requires external fixation initially, followed by definitive surgical repair once swelling subsides.
5. Stress Fractures / Hairline Fractures
It is commonly seen in athletes and military recruits, these are small cracks in the bone due to overuse or repetitive stress. It may get missed in initial X-rays. And require rest, bracing, and nutrition optimization. If ignored, can progress to full fractures
While less dramatic, untreated stress fractures can develop into full-blown breaks requiring orthopaedic surgery.
6. Special Mention: Right Tibia Fracture vs Left
While not a different type, the right tibia is dominant in most individuals. Recovery, driving, and functional rehab may vary based on which leg is injured.
Summary Snapshot of Types:
| Type | Location | Severity | Common Treatment |
| Tibial Shaft | Mid-leg | Moderate to severe | IM Nailing / Cast |
| Proximal Tibia | Near knee | High | ORIF Surgery |
| Distal Tibia | Near ankle | High | ORIF / External Fixator |
| Tibia-Fibula Combined | Full leg | Very high | Surgery |
| Stress Fracture | Any part | Low to moderate | Rest / Brace |
| Open Fracture | Any part | Critical | Emergency Surgery |
Symptoms, Causes & Diagnosis of Tibia Fractures
When Pain Is More Than Just a Fall
Most people don’t rush to the hospital after a slip or a bump. But when it comes to fractures of the tibia and fibula, hesitation can cost you months of mobility—or worse, permanent damage.
A tibia fracture, especially when combined with the fibula or involving the joint surface (like in proximal tibia fractures), comes with very clear warning signs. And if you’re dealing with any of the following symptoms after an injury, it’s a fracture until proven otherwise.
Clear & Definite Symptoms of a Tibia / Tibia-Fibula Fracture
- Severe, localized pain: Sudden, sharp pain in the lower leg or around the knee, often increasing with even slight movement
- Swelling and bruising: Rapid-onset swelling and discoloration along the shin or knee region
- Visible deformity: A crooked or misaligned leg shape strongly indicates a displaced fracture
- Inability to walk or bear weight: One of the most definitive signs — if you cannot put weight on the leg at all, suspect a tibia fracture
- Crepitus or cracking sound at time of injury: A clear sign of bone break
- Bone protruding through the skin (in open fractures)
- Numbness or tingling: May indicate nerve compression or vascular compromise, especially in high-impact injuries
What Causes Tibia and Fibula Fractures?
Tibia fractures are most often caused by high-energy trauma. But there are also specific causes tied to age, bone health, and activity level.
Common causes include:
- Road traffic accidents: The #1 cause in India. Direct trauma from bike, car, or pedestrian collisions.
- Falls from height: Especially in the elderly and construction workers.
- Sports injuries: Football, basketball, skiing, and gymnastics are high-risk sports for both shaft and proximal tibia fractures.
- Industrial or workplace trauma: Heavy objects falling directly on the leg.
- Twisting or rotational forces: Sudden twisting of the knee or leg in athletes or while walking on uneven surfaces.
- Osteoporotic bone fragility: In elderly individuals, even minor falls can cause fractures.
- Repetitive overuse: Runners and soldiers are prone to tibial stress fractures.
How Fractures Are Diagnosed?
Early diagnosis determines the type, location, complexity, and treatment pathway. Dr. MS Bajaj follows an orthopedic diagnostic process to ensure nothing is missed especially in cases involving the knee joint (proximal tibia) or soft tissue injury.
Clinical Examination
- Visual inspection, swelling, deformity, range of motion
- Palpation to check for tenderness and step-offs
- Neurovascular status check (pulse, sensation, capillary refill)
X-Ray (Radiographs)
- Standard AP (front) and lateral views
- Full-length tibia to include knee and ankle joints
- Helps confirm fracture line, displacement, angulation
CT Scan
- Especially critical for proximal tibia fractures and joint surface involvement
- 3D reconstruction gives surgeons a better roadmap for fixation
MRI Scan
- Used in cases with suspected ligament, meniscus, or cartilage damage
- Essential when soft tissue or bone marrow edema is present (seen in stress fractures)
- Bone Density Testing (if needed)
If you suspect a tibia fibula fracture, there is no debate. You need immediate evaluation by an orthopedic doctor in UP like Dr. MS Bajaj, who uses imaging and clinical expertise to determine the safest and best treatment, surgical or non-surgical.
Tibia Fracture Treatment in Uttar Pradesh, Ghaziabad, Indirapuram
- Tibia Fracture Treatment without surgery (Conservative) Management
- Tibia surgery
1. Non-Surgical (Conservative) Management
Used only for non-displaced, stable tibial shaft fractures or minor stress fractures. It is used mostly when fracture is closed, non-displaced, and well-aligned There is no joint involvement (e.g., not a proximal tibia fracture). Also the Patient who faced this is not a high-demand athlete or worker. No associated soft tissue, vascular, or nerve injury is found in this.
It Involves:
- Casting or bracing to immobilize the leg
- Non-weight-bearing for 6–8 weeks
- Follow-up X-rays every 2–3 weeks to ensure alignment remains
- Gradual physiotherapy after healing phase begins
Even in these seemingly “simple” fractures, the risk of malalignment or delayed union exists if follow-up is not strict. That’s why Dr. MS Bajaj closely monitors all conservatively managed patients.
2. Tibia Fracture Treatment Surgery for Severe Cases
Surgery is the right option when the patient has a displaced or unstable fracture or tibia and fibula both gets fractured or in case of Proximal tibia fracture (especially intra-articular / tibial plateau)
Other complex fractures like open fractures (bone protruding through skin) or comminuted fractures (multiple fragments) also need surgery based treatment. Common bone orthopaedic surgery treatment includes:
a) Intramedullary Nailing (IM Nail)
Most common surgical technique for tibial shaft fractures, a metal rod (nail) is inserted into the marrow canal of the tibia to stabilize bone from within. It is minimally invasive, preserves soft tissue and promote early weight-bearing in many cases.
b) ORIF: Open Reduction and Internal Fixation (Plates & Screws)
Best treatment for proximal tibia fractures (especially tibial plateau), involves open surgical exposure, realignment of joint surface, and fixation with custom plates. It allows for anatomical joint reconstruction, crucial for future mobility and arthritis prevention. But requires physiotherapy and controlled weight-bearing post-op during rehab.
c) External Fixation (Temporary or Definitive)
- Used in open fractures, polytrauma, or when soft tissue is badly damaged
- Metal pins or rods outside the body hold the bone fragments aligned
- Often used as first stage, followed by internal fixation once swelling reduces
Also useful in tibia-fibula fractures when both bones are shattered or when internal fixation is risky due to infection or tissue condition.
d) Minimally Invasive Plating (MIPO / LISS): It is thenewer technique used in complex proximal tibia fracturesthat combines stability of plate fixation with limited soft tissue disruption.It Helps reduce post-surgical pain, swelling, and scarring.
What Happens After Surgery?
Treatment doesn’t end in the OT. In fact, post-operative care and rehabilitation are just as important.
- Hospital stay: Usually 1–3 days depending on procedure
- Pain control & infection prevention
- Sutures/staples removed in 10–14 days
- Non-weight bearing initially → partial → full weight-bearing over 6–12 weeks
- Physiotherapy begins early (within days for joint mobility)
Most tibia and tibia-fibula fractures require surgery.
Conservative methods work only in stable, minor, and well-aligned injuries.
In joint-involved fractures like proximal tibia fractures, surgery is not just preferred—it’s necessary.
That’s why a right orthopedic surgeon early can make the difference between limping through life and walking pain-free with confidence.
Cost of Tibia Fracture Treatment in Uttar Pradesh, Ghaiabad, Indirapuram
| Treatment Type | Estimated Cost (INR) |
| Tibia fracture (non-surgical / casting) | ₹40,000 – ₹70,000 |
| Tibia shaft fracture with IM nailing | ₹1,30,000 – ₹2,00,000 |
| Tibia-fibula fracture surgery (ORIF) | ₹1,70,000 – ₹2,40,000 |
| Proximal tibia (tibial plateau) ORIF with plates | ₹1,95,000 – ₹2,70,000+ |
| External fixator (initial + final surgery) | ₹1,90,000 – ₹3,70,000 (total) |
| High-end implants (locking plates, LISS) | Add ₹50,000 – ₹95,000 depending on implant |
| Rehab / physiotherapy (3–5 months) | ₹2,000–5,000 per session |
These costs may vary based on city, room type, hospitalization days, post-op care, and implant brand.
Recovery & Rehabilitation: What to Expect Week-by-Week, Month-by-Month
People often ask, “Doctor, how long before I can walk again?” The truth is: recovery after a tibia or tibia-fibula fracture can not have fixed date as it is a progressive process.
General Healing Timeline
- Hairline / stress fractures: 6–8 weeks with bracing and offloading
- Simple, non-displaced fractures: 10–12 weeks
- Tibia-fibula fractures with surgery: 16–24 weeks
- Proximal tibia (tibial plateau) fractures: 5–6 months minimum
Recovery Stages – What Happens at Each Phase
Phase 1: Weeks 0–3: Aims to protect the injury, manage swelling, prevent muscle wasting.Immobilization in cast or post-op brace is important.Mostly the leg is kept elevated, ice therapy to reduce swelling is considered.Strict non-weight bearing is must.
Pain control + monitoring wound healing (if operated) Proximal tibia fracture patients often wear a knee immobilizer or hinged brace locked in extension.
Phase 2: Weeks 4–8: The idea is to promote bone healing, prevent stiffness, and start gentle activity.X-rays taken to confirm callus formation / alignment. Patient can start partial weight-bearing (as permitted) with walker/crutches.Hinged brace unlocked gradually for knee ROM (for tibial plateau fractures)
Phase 3: Weeks 8–12: Controlled loading, strengthening, gait re-training withgradual increase to 50–75% weight-bearing (guided by bone specialist).Strengthening for quads, hamstrings, glutes starts withgait correction, walking with single crutch or cane.
Phase 4: Weeks 12–20: Regain full weight-bearing, improve endurance, restore normal motion.Full weight-bearing without assistive devices can be expected.Return to desk job/work possible by this stage for most but high-impact activities still avoided
Phase 5: Month 6 and Beyond: Return to normal function and sports
What Slows Down Recovery?
- Smoking or poor nutrition
- Osteoporosis
- Diabetes or vascular conditions
- Ignoring rehab protocols
- Improper surgical alignment or infection
- Psychological fear of reinjury
This is why a trusted orthopedic doctor like Dr. MS Bajaj is needed to focuses on the operation and supervise post-op care personally.